Polycystic kidney disease, and future drugs that might treat it
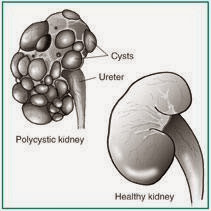
Earlier, we had talked about kidney cysts, and how they could be present in different disease conditions of varying severity. Lets talk a little about one specific entity characterized by multiple cysts in the kidney, called Polycystic Kidney Disease (PKD), and some potential treatment options that might pan out in the future.
PKD is one of the most common genetic disorders, affecting as many as 1 in 500 people. It is a leading cause of kidney failure. It occurs because of mutations in certain genes that are present on different human chromosomes. These genes could be either PKD1, PKD2, or PKD3 genes. Which of these genes has the mutation and what type of mutation it might be, has a huge effect on the expected outcome of PKD. It could mean a difference between a patient developing kidney failure at the age of 49 versus 79 years! A discussion of the different types of mutations is beyond the scope of this blog.
Typically, the mutation is present at birth. However, cysts might not be apparent at that time. These cysts grow into appreciable fluid filled sacs over the first couple of decades, at which time they may begin to cause symptoms or signs. Most people who know of a family history of PKD have a low threshold of being diagnosed with PKD since both patients and physicians are well aware of the strong familial nature of the disease. Sometimes however the family history might not be known, or it could be a case where the parent had a relatively benign version of the mutation where the disease might not have caused kidney failure till the late 70s. In this case, the affected parent could have died before the disease ever had the chance to progress to end stage kidney disease.
The diagnosis is usually made when cysts are picked up on imaging studies. However, just because someone has multiple cysts in the kidneys does not necessarily mean that they have PKD. It could just be a case of one-too-many "simple" cysts and other possibilities that we had discussed earlier. This is a common clinical conundrum that I have faced in my practice as a nephrologist, and this could necessitate genetic testing.
ROLE OF ADH
As much as I want to not make this blog too technical for the average reader, I will have to make a mention of a hormone called ADH, or the Anti Diuretic Hormone (also known as Vasopressin) that is produced by the pituitary gland. This is a hormone that acts on the kidney and makes it retain water. It is what makes the urine look dark and concentrated when you have not had enough water, or spent a day outside in the hot sun. If it weren't for ADH, a day on the beach would tantamount to a life threatening experience where you would dehydrate yourself to death within a matter of hours. It is the hormone that has helped life evolve from the oceans to land, eons ago. If it weren't for ADH, you and I would be ocean dwelling organisms, unable to withstand the harsher dehydrating influence of a hotter land surface under a blazing sun!
So why am I talking about ADH? Well, studies have shown that ADH is one of the factors involved in the growth of the cysts (the reason for kidney failure) in PKD. In other words, if you could somehow inhibit the action of ADH on the cysts and consequently slow down cyst growth, you could possibly stem the inexorable progression of PKD.
 |
| Courtesy http://kidney.niddk.nih.gov/kudiseases/pubs/polycystic/ |
TYPICAL TREATMENT CURRENTLY AVAILABLE
One of the most frustrating things in clinical nephrology is to give a diagnosis of PKD to a young patient, and follow that up by saying that they could progress to end stage renal disease requiring dialysis, and “there is not much I can offer to change that”.
In the absence of specific treatments on the market, we are limited to managing the complications of PKD. These include high blood pressure, kidney infections, kidney stones, abnormal electrolytes etc. High blood pressure is treated using specific medications called ACE inhibitors or ARBs. Often, nephrologists will also recommend that patients drink as much as 3 liters of water daily. This possibly helps with minimizing the risk of kidney infections and stones. But more importantly, it actually lowers ADH levels too! As we discussed above, ADH levels will go up anytime you are losing water/dehydrated. That spike in ADH levels could theoretically quicken cyst growth and kidney failure. Hence, keeping ADH levels low by optimizing water intake could slow down progression of PKD.
FUTURE TREATMENTS THAT MIGHT BE MORE EFFECTIVE
Could we then inhibit the action of ADH on the kidney and prevent cysts from growing? Enter tolvaptan, a medication that was originally approved for treatment of low sodium levels. Recently, the well-publicized TEMPO trial has shown a potential clinical application for tolvaptan in stemming the progression of PKD by slowing the growth of the total kidney volume and GFR decline over a 3-year period.
Another agent that is being studied for a few years for a potential role in inhibiting cyst growth in PKD is a drug called octreotide (a long-acting synthetic version of a hormone called somatostatin). This is an agent that we in the nephrology universe have been using for some time for the treatment of hepatorenal syndrome, a type of combined liver and kidney failure. A trial had first reported in 2005 that a 6-month treatment with somatostatin could slow cyst growth. Although we know that decline in kidney function in PKD follows cyst growth, the study stopped short of saying that slowing the cyst growth in this case would translate in to clinically meaningful kidney protection. Then, a few months ago we saw the results of the ALADIN trial (this is officially my vote for the "coolest sounding medical study of the year" award!) published in the Lancet. This study had a longer follow-up period than the previous studies, and indicated a significantly lower kidney volume in patients treated with octreotide at 1-year follow-up, but not at 3-years.
Given the data we have so far, it appears that octreotide could have a potential role in the treatment of PKD. For some reason, it appears that octreotide slows growth in kidney volume over one year, but the effects become insignificant over the long term. Obviously, more comprehensive studies looking at long-term hard outcome data are needed. Another interesting thing would be to compare the data for octreotide vs. tolvaptan.
Although both these agents have shown promise so far (in addition to other contenders like mTOR inhibitors), a major concern is cost. All other things being equal, octreotide could be a cheaper alternative than tolvaptan for what essentially could be a lifelong treatment. At my time of writing this, a ten-day course of 15 mg tolvaptan pills was priced at $3440.00, while a 100 mcg octreotide injection was priced at $11.93!
A more comprehensive database of up-and-coming drugs that might be the magic cure for PKD is available here. I can’t wait for the day when we will be able to offer our patients something more definitive for treatment of PKD rather than the current “bandaid” regimen of ACE inhibitors, increased water intake, etc.
Veeraish Chauhan, MD, FACP, FASN
Nephrologist
Bradenton / Sarasota, FL


Comments
Post a Comment