Diet for patients with kidney disease: A little sweet, a little salty, and what to eat more/less of?
You are what you eat. Your kidneys are no different. Diet and lifestyle have a huge influence on the development of kidney disease, as well its rate of progression once it develops. Hence, in my practice, and especially in patients with early stage chronic kidney disease (CKD) or stage 3/early stage 4, I place a strong focus on diet (in addition to treating the cause of CKD) which may sometimes go a long way in preventing disease progression. This does not mean that the right diet is not important in advanced stages of CKD. It very well is; however, you will probably need more aggressive medical management in those stages. I have emphasized before that, like many other things in life, prevention is not only better than cure, it is much much easier too. Once GFR (glomerular filtration rate, a measure of your kidney function) permanently declines, it is unlikely that it will increase. Hence GFR decline is often a "one way highway".
1) So the answer to the question, "why I need to eat right" is straight forward. Eat right, and you can help slow your CKD. The tougher question is, "what do I eat"? Most patients with CKD have a lot on their plate anyway, in terms of their disease burden. The typical CKD patient seen in the clinic is a diabetic/hypertensive older person. You would probably be already aware of some dietary restrictions for your other diseases. For instance, diabetics are well aware of the importance of limiting foods that are high in sugar. This is important from a kidney perspective as well. We have a ton of evidence out there that shows that good blood sugar levels (called "glycemic control" in medical parlance) decrease the chances of you developing diabetic kidney disease, and reduce the risk of death even in patients who already have advanced CKD or are on dialysis.
2) I started this discussion with diabetes and sugar intake, and its influence on CKD, because diabetes is the single most common cause for the development of end stage kidney disease requiring dialysis. But, lets talk for a moment about the other big culprit; salt, or more specifically, sodium. Sodium intake has a huge influence on blood pressure, even more so in patients with kidney disease. A recent British Medical Journal study got a lot of attention in popular press when it reported that reducing recommended daily dietary salt intake by 50 percent could save 100,000 deaths from heart attack and stroke in the United States every year! I can well see salt intake becoming the next big public health issue across America after New York Mayor Michael Bloomberg made it his newest health initiative. Leaving the politics aside, suffice it to say that the National Institute of Health (NIH) recommends limiting daily sodium intake to 1500 milligrams if you have or are at risk of kidney disease. Please note, we are talking about sodium, and not salt intake. Typically, salt, or sodium chloride, is the most common source of dietary sodium. However, one could end up getting sodium from other sources like baking soda (sodium bicarbonate) which also counts towards that 1500 mg limit.
Many patients tell me that they "don't add any sodium/salt to their diet". However, when I test their urine to approximate their daily sodium intake, it is often high. This is because most of this 1500 mg, as high as 80%, is already present in the food that you eat, even if you don't add any extra salt to it. So it goes without saying that to control your sodium intake, you would probably need to be obsessive about reading the food labels and seeing how much sodium there is in a serving. As a rule of thumb, anything with more than 300 mg of sodium per serving (or 20%) qualifies as a "high sodium" food and should be limited accordingly. The usual culprits in the high sodium category include canned foods/meat/fish, pizza, chips, ketchup, sauces, salad dressings, noodle soups, processed cheese, etc.
The battle against sodium is not easy to win. Which is why I used the word "obsessive" in the above paragraph to describe what quality you will need to possess to stay within the recommended limit. The other day, I decided to try this on myself first hand. On a weekly shopping errand (not my favorite activity!) that my wife sent me on to, I carefully made my way through the aisles of a popular supermarket here in Florida. Here are a few pictures of what the food labels in the sauces and salt sections revealed (please note that this is not an endorsement or criticism of a particular brand of food item, just a revelation of facts):
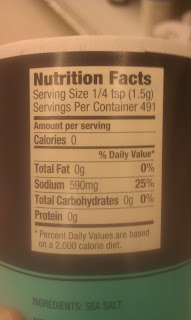 |
| Sea Salt: you can see that it has just under half of the recommended daily sodium intake in 1/4 tsp! |
 |
| Garlic salt does a little better than sea salt having less than half of sea salt's sodium, pound for pound |
 |
| An example of a popular "salt substitute" with no sodium. However, this has potassium which may be a problem if you have advanced CKD when even potassium intake will need to be restricted |
 |
| Salad dressing with over 300 mg of sodium in one serving |
 |
| Mrs. Dash- My personal favorite solution to flavor food with spices and herbs. No worries about either sodium or potassium! |
Needless to say, educating oneself and being mindful of the facts on the food label is the first step in winning the battle against sodium. You could try and flavor your food with spices or herbs instead. Most patients crave salt in the initial days, but don't miss it if they can make it through the first few weeks! If you eating canned food, rinse it before you consume it.
3) The other essential food component that could have a bearing on your kidney function is your protein intake. There is scientific evidence to support the consumption of particular kinds and amount of protein. Plant protein (grains, nuts, etc) might be better than animal protein. This is because the amount of acid load is more in animal protein, which might be an important factor in worsening CKD, especially in the advanced stages. Finally, red meat could be a big source of uric acid, which has been shown to be associated with worsening of CKD. Certain high quality protein foods may have less phosphorus (something that needs to be limited in advanced CKD) and could be better than other sources.
The amount of protein you eat is crucial as well. Both high and low intake have repercussions, including worsening of CKD/blood urea levels, and malnutrition, respectively. The recommended daily intake is about 0.8 to 1 gram of protein per kilo body weight. It is hard for the average person to sometimes estimate what this amount means in real world terms (that is, how much fish or eggs or beans you could eat), as well as which foods might be a better qualitative source of protein that others. For these reasons, it might be a good idea to see a dietitian to help you come up with a customized diet plan.
4) You also need to watch your potassium and phosphorus intake in advanced stages of CKD. Lastly, lets not forget the common sense advice that we have heard so many times before. Limit your fat/cholesterol intake, don't deep fry foods if you can help it, grill your food, etc, etc. The reason is simple. Most patients with kidney disease eventually die from heart or vascular disease! So you still need to work on keeping your heart and blood vessels healthy.
I understand that it is not easy to practice and keep track of so many food restrictions, BUT, it is possible. You will most likely need the help of a dietitian though. We luckily live in times when we do have alternative food items with the right amount of sodium/sugar/protein/potassium/phosphorus/uric acid available! This is far removed from those dreaded days when treatment for kidney failure included putting patients on an extremely low protein/potassium/phosphorus foods, referred to as the "cardboard and pepper diet"!


Great info! Love the way you have given practical information to make the changes necessary.
ReplyDeleteThank you!
Deletegreat info, cheers
ReplyDeleteThanks Chris!
DeleteBeen having some kidney issues and I found your blog. Great information! Thanks for posting it.
ReplyDeleteThank you!
Delete